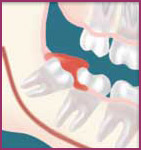
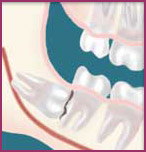
Wisdom TeethWisdom teeth, officially referred to as third molars, are usually the last teeth to develop. They are upper and lower teeth whose function is to grind food as part of the digestive process. They are located in the very back of your mouth, next to your second (or twelve year) molars and near the entrance to your throat. They usually complete development between the ages of 15 and 20, a time traditionally associated with the onset of maturity and the attainment of Wisdom. Why Should I Have Them Removed?Although people develop and grow 32 permanent, adult teeth (16 in the upper and 16 in the lower jaw), most do not have enough room in their mouth for all of these teeth to completely erupt. Since the wisdom teeth are the last to develop, they often will not have enough room to adequately erupt into the mouth to become fully functional and cleanable teeth. This lack of room or space can result in a number of harmful effects on your overall dental health. When this occurs they are said to be impacted, indicating their inability to erupt into an alignment that will allow them to be able to function in the chewing process. There are several types of impactions:
If you do not have enough room in your mouth for your third molars to erupt and they become impacted, several detrimental results can occur:
Unless you have an active problem at the time of your consultation, the reason for removal is primarily preventative to avoid long-term problems. There is a lower chance of complications and long-term problems if wisdom teeth are removed before they start to hurt. By the time wisdom teeth become symptomatic, damage may have already occurred. We will need to see you for a consultation before it is determined if you will benefit from wisdom tooth removal. We will need to take a special x-ray of your mouth and jaws to determine how much room you have, if any, for your wisdom teeth to erupt. So, Do I Really Have To Have Them Removed? In most cases the absolute answer is no. Unless you have been told that you have a life-altering disease process (which is unlikely), you don't have to do anything until or unless YOU chose to do so. This is not critical, life-saving, emergent medical treatment. It is elective. We understand, however, that we can identify problematic patients early in their teens and treat them when the impact of the surgery is minimal and their ability to recover is at its maximum. That is the Best Age to have them removed? If it is recognized that you do not have enough room in your mouth for your third molars to erupt, it is advisable to have them removed as soon as it is recognized. In some patients it is as early as 11 or 12 whereas in others it may not be until 17 or 18 years of age. You will heal faster, with more predictable final healing, and have fewer complications that an older patient. An x-ray of the jawbone will allow us to evaluate root formation and determine the optimum time for wisdom tooth removal. What If I Don’t Have Them Removed Now? Many people, especially in years past, were told to take a "wait and see" approach to wisdom teeth. Many who did not have adequate room developed localized problems previously mentioned. The problem with this approach is that if it is necessary to remove impacted wisdom teeth in your twenties, thirties, and forties or beyond, it is clearly more difficult for you as the patient. The post-operative course is usually prolonged and there is a higher complication rate. Treating these complications is more difficult than with a younger patient. If you do not have your impacted wisdom teeth removed in your teenage years or early in your twenties, it may be advisable to wait until or unless a localized problem (such as cyst formation or localized gum disease and bone loss) develops and then treat the affected area only. This is because the predictability of healing decreases with age and the likelihood of infection and delayed healing increases. If I Decide to Do It, When Should I Have Them Removed? There is probably never a good time to undergo an elective procedure such as wisdom teeth removal. We recommend that the surgical appointment doesn’t conflict dramatically with school activities. The most ‘popular’ time for wisdom teeth removal is during the summer and school vacations. If you live at or near home, any time you have a long weekend is also good. The bottom line is that with adequate preparation, any time will work for most people if they have planned accordingly in advance. What Happens On The Day They’re Removed? First of all, you need to decide if you want general anesthesia ("go to sleep"). Most people clearly prefer to be unaware of the experience when they have their wisdom teeth removed. You will be provided with appropriate anesthesia options for you at your consultation. On the day of your procedure, you will take medications to help minimize post-operative pain and swelling. We ask that a parent or responsible adult accompanies you to the office and plans to stay with you the rest of the day. Your procedure will take about an hour and you will probably be in the office for 1 to 2 hours. Our staff will review your post-operative instructions. When you leave the office you will be comfortable and drowsy. Most patients prefer to go home and rest with no other physical or scholastic activities planned for a few days. All outpatient surgery is performed under appropriate anesthesia to maximize your comfort. We have the training, license, and experience to provide various types of anesthesia to allow patients to select the most appropriate alternative. These services are provided in an environment of optimum safety, utilizing modern monitoring equipment and staff experienced in anesthesia techniques. What Happens Afterwards — What Will I Feel Like? Most of the time you will want to maintain a low profile for a few days. We ask that you follow your post-operative instructions closely as they will make you most comfortable during the first few days following your procedure. Please allow the time to let your body begin healing before resuming an active social, academic, or athletic schedule. Most patients feel like they are over the hump in 3 to 5 days. Are There Any Problems? Temporary problems you may experience in the postoperative period include stiffness of the jaws or jaw joints, chafing around the corners of your lips, facial bruising, or oozing from the extraction sites. The postoperative instruction sheet we will provide should answer many of the questions related to these more common concerns. If not, don’t hesitate to call the office. As with any surgical procedure there is the possibility that infection can occur postoperatively. This usually requires an office treatment visit. Occasionally, you may experience the following: postoperative numbness in your lip, chin or tongue, involvement of your sinuses, or damage to an adjacent tooth. Dr. Imbeau will review these in greater detail during your consultation appointment. What are Dry Sockets? Dry sockets continue to be a common problem people experience following dental surgery. They arise due to premature loss of a blood clot in the empty tooth socket. This seems to occur with greater frequency in people who smoke or are taking birth control pills. Recent studies have linked smoking and hormone therapy with increase risk of clotting. Clots that form without a valid reason can disrupt blow flood in the small blood vessels of the jawbone. If the bone surrounding the teeth is blood starved, it may undergo chronic damage due to lack of proper nutrition of the bone cells and reduce it's ability to recover from trauma, surgical or otherwise. While both jaws can be affected, they occur more frequently in the lower jaw on the third to fifth day. They cause a deep, dull, continuous aching on the affected side(s). Patients may first notice the pain starting in the ear radiating down towards the chin. It frequently begins in the middle of the night, and mild pain medication usually doesn’t help. Treatment involves placing a medicated dressing in the "empty" tooth socket. This will help decrease the pain (usually within 20 minutes) and protect the socket from food particles. The effectiveness in alleviating the pain lasts for 48 to 72 hours. The medicated dressings may be replaced more than once. The dressing doesn’t aid in healing. The only reason to place a dressing is for pain control. If NurofenŽ (ibuprofen) is controlling the pain, the socket will heal without a dressing. An irrigation device may be given to you to help keep food particles from lodging in the extraction site following removal of the dressing. If you think you have a dry socket, contact the Centre so that Dr. Imbeau can assess the situation and provide the necessary care. If you have a tendency for dry sockets, it is recommended that a further assessment of the jawbone density and quality be performed. This will involved a more detailed examination and medical history to assess if you have a greater susceptibility for a condition called hypercoagulability. Hypercoagulability is characterized by an increase tendency to form clots when normally they should not and also a reduced ability to break down the clots as quickly as they should. Mild hypercoagulability, while not enough to cause major problems, is enough to impede normal under certain conditions. Special x-rays and ultrasound bone scans may also be recommended. Even if the gum closes over a poorly healing socket, it does not mean that the bone inside will heal properly. Poorly healing socket can lead to poor bone density ( osteoporosis ) in the affected area which in turn increases the risk of developing a condition called ischaemic osteonecrosis.
What Does It Cost ? Because of the different types of impacted wisdom teeth, along with different anesthesia options, it is impossible to give you a realistic estimate of what our services will cost until we have reviewed your x-rays. What If I Have Questions Before Surgery? We recognize that having your wisdom teeth out is NOT something you really want to do. We also realize that with an active schedule there is never a really good time to have this done. If this information, combined with information you receive at your consultation appointment doesn’t answer all of your questions, please call the Centre to speak to our Clinical Coordinator. |
 room
to allow the gum tissue to recede to allow
adequate cleaning of the tooth.
room
to allow the gum tissue to recede to allow
adequate cleaning of the tooth.